If a clinician recommends root canal therapy for a troubled tooth, there’s no reason to panic. Modern endodontic care is predictable, gentle, and focused on relieving pain while preserving natural teeth whenever possible. In many cases a root canal is the most effective way to stop an infection, end lingering toothache, and keep your smile intact.
At the office of William L. Krell, DDS, MAGD, our approach combines proven techniques with contemporary technology to deliver precise, comfortable treatment. Patient comfort, clear communication, and long-term function are the priorities that guide every decision we make during diagnosis and treatment planning.
Keeping a natural tooth whenever possible preserves the way your jaw functions, supports nearby teeth, and helps maintain facial structure. A properly treated and restored tooth typically performs like any other tooth and lets you chew, speak, and smile without the adjustments required by a replacement.
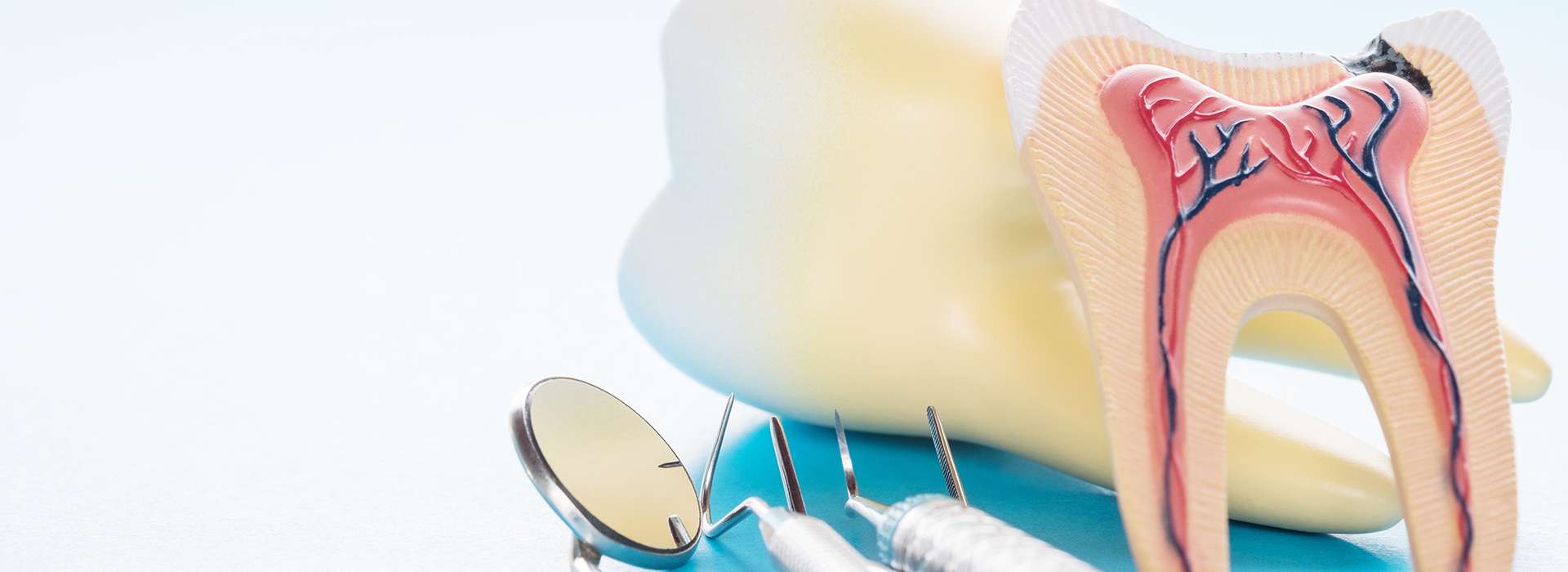
Root canal therapy removes the damaged or infected internal tissues while leaving the outer tooth intact. When followed by an appropriate restoration — often a crown — the treated tooth regains strength and can provide many years of dependable service. This conservative approach prioritizes saving tooth structure over extraction whenever clinically feasible.
Success rates for contemporary, non-surgical root canal treatment are high when cases are properly diagnosed and restored. Combining careful treatment techniques with modern materials and follow-up care gives most treated teeth an excellent long-term prognosis.

Inside each tooth is a soft core of connective tissue, nerves, and blood vessels known as the dental pulp. That tissue keeps the tooth alive during development and provides sensory feedback throughout life. When decay, trauma, or repeated restorative work breaches a tooth’s protective outer layers, bacteria can invade the pulp and trigger inflammation or infection.
Infection can progress down the root canals and reach the bone surrounding the root tips. At that stage, the problem may cause localized bone loss and produce symptoms ranging from mild sensitivity to severe, throbbing pain. In some cases the pulp dies and the tooth becomes non-vital without causing obvious symptoms, which is why careful examination and imaging are important.
Understanding how and why the pulp becomes affected helps explain why root canal therapy is often the preferred treatment: removing the source of infection and sealing the internal spaces of the tooth prevents further damage and preserves the tooth’s role in the mouth.
Some problems announce themselves clearly: persistent tooth pain, especially pain that wakes you at night or that intensifies with biting, should prompt an evaluation. Heightened sensitivity to hot or cold that lingers after the stimulus is removed is another common early warning sign of pulpal inflammation.
Other indicators include visible changes to a tooth — darkening or discoloration can signify internal damage — and evidence of physical compromise such as a chip, crack, or fracture that exposes the inner tissues. Swelling of the gum near a tooth or a persistent bad taste can indicate an abscess that requires prompt attention.
Some affected teeth show little or no pain but reveal problems on routine X-rays or during a dental exam. Regular dental visits help identify these quieter issues early, which often allows for more straightforward and successful treatment.

A typical visit begins with a careful clinical exam and radiographs to map the tooth’s anatomy and the extent of any infection. Local anesthesia numbs the area so the procedure is comfortable; additional sedation options are available for patients who experience anxiety.
Your dentist will create a small opening in the crown of the tooth to access the pulp chamber, then gently remove the inflamed or infected tissue. The canals are cleaned, shaped, and disinfected with specialized instruments and irrigation solutions, then filled with a biocompatible material to seal the internal spaces and prevent reinfection.
Some teeth can be treated in a single appointment, while others require two visits, particularly when active infection needs time to resolve. After the root canal procedure is complete, a durable restoration — commonly a crown — is recommended to protect the tooth and restore full function.

After treatment you can expect some tenderness or mild inflammation around the treated tooth as the surrounding tissues heal. Numbness from anesthesia will wear off within a few hours; any discomfort is usually manageable with over-the-counter pain relievers or medications prescribed when appropriate.
It’s important to protect the treated tooth while it’s being restored. A temporary filling is often placed after therapy, but until a permanent crown or definitive restoration is seated the tooth can be more vulnerable to fracture. Your dentist will advise on timing to complete the restoration and restore normal chewing forces.
With proper restoration and routine oral hygiene, a tooth that has undergone root canal therapy can remain functional for many years — often a lifetime. Regular dental checkups help ensure the treated tooth and surrounding tissues remain healthy and that any concerns are addressed promptly.
At the office of William L. Krell, DDS, MAGD, we focus on clear communication, careful technique, and thoughtful follow-up to help patients navigate root canal treatment with confidence. If you have questions about symptoms you’re experiencing or would like more information about endodontic care, please contact us for a consultation and evaluation.
A root canal procedure is the best way to save a tooth that has been damaged by decay or injury and preserve your natural smile. The alternative is an extraction and treatment to replace the tooth. While at times a tooth is non-restorable and an extraction is the only option, when possible, it’s best to try and save your natural tooth. With proper care, a tooth with root canal therapy can serve your smile well for many years to come.
Despite lingering myths from before the age of modern dental anesthesia and technology, having a root canal procedure today is as routine and comfortable as visiting the dentist for a filling. While the procedure is performed under local anesthesia with your tooth completely numbed, we can also discuss options in dental sedation.
Whether the symptoms of a dental infection subside after a course of antibiotics, a draining abscess provides you with some temporary pain relief, or a tooth with radiographic evidence of pathology has not yet developed symptoms, it’s essential, before an infection worsens or occurs, to have a root canal procedure performed. In this way, the tooth can be disinfected, filled, and sealed to protect your health and avoid further problems.
If you have sustained a dental injury, have a toothache, jaw pain, swelling, or are experiencing any other unusual and uncomfortable oral symptoms, contact our office immediately for care. Dental problems that have not been evaluated and treated can significantly worsen, producing more severe damage and consequences for the involved teeth, your oral health, and even your overall wellbeing. Once you get in touch with our office, our friendly and compassionate office team will get you in for care at your earliest convenience.
While some root canal procedures can be completed in one visit, others may involve 2 or 3 appointments. How long it takes depends on various factors, including active infection, the number of canals in the tooth, and the tooth’s location or anatomy.
With a success rate that exceeds 95%, root canal therapy remains the most effective procedure to save a tooth in which the inner vital tissues have been damaged. However, as with all healthcare procedures, there are a small percentage of cases where the teeth become symptomatic a second time. The good news is that many of these teeth can still be saved with root canal retreatment or a minor surgical procedure known as an apicoectomy.
The best ways to maintain a tooth with root canal therapy are to get the proper restoration required to rebuild and protect the tooth, maintain proper oral hygiene, and schedule appointments for routine dental checkups and care.
Saving a tooth with root canal therapy is a wise investment that, in the long run, is typically less costly and invasive than having the tooth extracted and replaced with a fixed bridge or implant. As far as the exact cost of care, it can vary depending on which tooth is being treated. Many dental insurance plans provide coverage for root canal therapy. At the office of William L. Krell, DDS, MAGD, we do our best to optimize your dental benefits and minimize your out-of-pocket expenses. Our staff will answer all your questions about the cost of care and discuss all your payment options.
At the office of William L. Krell, DDS, MAGD, we use the latest technology and most effective methods of care to provide precise and gentle care. Our reputation for excellence is based upon a consistent record of achieving successful treatment outcomes while providing prompt, stress-free, and convenient treatment for every type of dental need.
A root canal is a dental procedure that removes diseased or injured pulp from inside a tooth. The pulp contains nerves, blood vessels and connective tissue that can become inflamed or infected after deep decay, trauma or repeated dental work. Removing the pulp and sealing the internal spaces eliminates the source of infection and preserves the tooth's structure.
Root canal therapy focuses on saving a natural tooth rather than extracting it and replacing it with an implant or bridge. When combined with an appropriate restoration, a treated tooth can continue to perform normally for many years. Modern techniques make the procedure predictable and reliable for most cases.
Common signs that a tooth may need root canal treatment include persistent or severe toothache, sensitivity to hot or cold that lingers, and pain when biting or chewing. Noticeable changes such as darkening of a tooth, a visible crack, or swelling at the gumline also warrant evaluation. A persistent bad taste or drainage near a tooth can indicate an abscess and should be assessed promptly.
Some infections develop without obvious symptoms, so problems are sometimes first detected on routine X-rays or during an exam. Your dentist will combine clinical findings and radiographic imaging to determine whether the pulp is compromised. Early diagnosis generally allows for simpler, more successful treatment.
A typical root canal appointment begins with a clinical exam and radiographs to map the tooth's internal anatomy and the extent of infection. Local anesthesia numbs the area so patients are comfortable throughout the procedure. The dentist accesses the pulp chamber through a small opening in the crown and gently removes inflamed or infected tissue. These steps are performed with specialized instruments and irrigation to disinfect the canals.
Once cleaned and shaped, the canals are filled with a biocompatible material to seal them against reinfection. Some teeth can be treated in a single visit while others require two appointments when infection needs time to resolve. Afterward a final restoration, often a crown, is recommended to protect and strengthen the tooth.
Most patients report little to no pain during root canal therapy because modern local anesthesia and techniques are highly effective. For those with dental anxiety, additional sedation options can be discussed to increase comfort and reduce stress. The procedure itself is focused on removing the source of pain, so many people experience relief once infection is controlled. Your provider will communicate each step to help you feel informed and relaxed.
Mild soreness or tenderness around the treated tooth is common for a few days as tissues heal and inflammation subsides. Over-the-counter analgesics or prescribed medications can manage discomfort when needed. Contact the office if you experience increasing pain, swelling, or persistent numbness.
Initial recovery usually takes a few days, during which time you should expect gradual improvement in comfort and function. Numbness from anesthetic resolves in a few hours and any sensitivity should lessen as healing progresses. If pain or swelling persists beyond several days, your dentist will evaluate the tooth and surrounding tissues.
Until a permanent restoration is placed, avoid biting directly on the treated tooth and follow any dietary recommendations from your provider. Maintain good oral hygiene by brushing and flossing carefully around the temporary restoration to prevent new decay. Attend scheduled follow-up visits so the tooth can be restored and monitored for long-term success.
Contemporary, non-surgical root canal therapy has high success rates when cases are appropriately diagnosed and restored. Factors that influence prognosis include the extent of infection, the tooth's anatomy, and timeliness of treatment. Careful technique, quality materials, and proper restoration all contribute to favorable outcomes.
A well-treated and restored tooth can remain functional for many years and often a lifetime with routine care. In some instances retreatment or endodontic surgery may be needed if symptoms recur or persistent infection is detected. Regular dental examinations and X-rays help detect issues early and protect the longevity of the tooth.
The primary alternative to root canal therapy is extraction followed by an appropriate tooth replacement, such as a dental implant or bridge. Extraction removes the infected tooth but does not address the bone-preserving benefits of keeping a natural tooth when possible. Replacement options restore function and esthetics, but each has different clinical considerations.
Your dentist will discuss the condition of the tooth, surrounding bone, and overall oral health when recommending treatment. When a tooth can be predictably saved and restored, preservation is generally preferred to maintain natural jaw function. In cases of severe structural damage or non-restorable teeth, extraction becomes the appropriate choice.
A crown is commonly recommended after root canal therapy because teeth can become more brittle once the pulp is removed. Crowns help redistribute chewing forces, protect the remaining tooth structure, and reduce the risk of fracture. The type of restoration depends on the tooth's location, amount of remaining structure, and functional needs.
Some posterior teeth with minimal structural loss may be restored with onlays or composite restorations, while front teeth may require less extensive coverage. Advances like same-day CEREC crowns can streamline the restoration process when clinically appropriate. Your dentist will explain the restoration options and timing to achieve the best long-term result.
Modern technology improves both diagnosis and treatment of root canal problems by revealing details that were once difficult to see. Tools such as cone-beam computed tomography (CBCT), digital radiography, dental operating microscopes, and rotary instrumentation enhance precision and detection of complex anatomy. These advances help clinicians plan treatment more accurately and reduce the risk of missed canals.
Improved imaging and instrumentation also help limit unnecessary removal of tooth structure and focus disinfection on affected areas. Better visualization and materials can shorten treatment times and improve predictability. When technology is combined with experienced technique, patients benefit from more conservative and successful care.
At the office of William L. Krell, DDS, MAGD, patient comfort and clear communication are central to our approach to root canal therapy. We use effective local anesthesia, offer sedation options for anxious patients, and take time to explain each step of treatment. Our team coordinates follow-up care to ensure healing proceeds smoothly and concerns are addressed promptly.
Before treatment we review medical history and imaging so you know what to expect and how to prepare. During recovery we provide specific aftercare instructions and are available to answer questions by phone or during follow-up visits. Personalized attention and evidence-based techniques help patients navigate treatment with confidence.

Get in touch with us today!